The Case for Increased Ventilation
Employees reporting to or remaining at work despite illness, a practice known as “presenteeism,” can have serious repercussions. Not only do sick employees tend to operate at less than their usual level of performance, they risk infecting others (see sidebar). The impact on a company's bottom line can be devastating; the total cost of presenteeism to U.S. employers is an estimated $150 billion to $250 billion a year and rising.3
In plans to curtail employer health costs, finding direct disease reduction or facilities improvement can be difficult. Often, health-cost containment is viewed as an administrative matter, with efforts focused postinfection. Managers assume ventilation standards fully cover indoor-health issues when, in fact, they specify the least amount of air required to keep buildings habitable and safe.
Facilities managers have at their disposal a proven and effective means of helping to contain employer health costs: increasing ventilation. This article will discuss how increased ventilation can prevent the spread of disease among workers in commercial and government office buildings.
Costs
The conditioning (cooling, dehumidifying, heating, and filtering) of fresh outside air is considered costly by most facility engineers. Compared with the conditioning of recirculated indoor air, it is. But when sick-leave costs are thrown into the mix, the conditioning of fresh outside air does not seem so expensive.
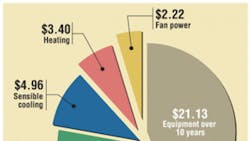
For instance, providing the ANSI/ASHRAE Standard 62.1, Ventilation for Acceptable Indoor Air Quality-required 20 cfm of fresh air for one office worker for one year in Jacksonville, Fla., costs $48 (Figure 1). That includes upsized-equipment costs of $2,000 per ton, spread over the equipment's 10-year life; electricity costs of 12.5 cents per kilowatt-hour; and fuel-gas costs of $1.25 per therm. Compare that with the annual sick-leave cost of $1,580 for one government employee or $478 for one private-sector employee. If doubling the ventilation rate could cut sick-leave costs in half — in a 1994 test, Polaroid Corp. doubled (from 25 cfm to 50 cfm) ventilation rates in 40 buildings (3,720 workers), achieving a 53-percent sick-leave decrease4 — the economic return would be at least fivefold. (Breaking even would require a reduction of sick-leave costs of just 10 percent.) Greater productivity attributed to reduced presenteeism and lower health-insurance costs attributed to fewer and/or less-costly claims makes increased ventilation even more compelling.
Increased ventilation is estimated to save the U.S. economy $6 billion to $14 billion in respiratory-illness costs, $1 billion to $4 billion in allergy and asthma costs, and $10 billion to $30 billion in sick-building-syndrome- (SBS-) symptom costs.5
The Power of Prevention
Although considerable research concludes higher air-exchange rates (AERs) lead to absenteeism reductions and productivity improvements (Figure 2), engineers tend to focus solely on the fact that, with rare exception, higher AERs lead to higher energy costs.
After doubling the amount of outside air supplied to 40 of its buildings, Polaroid Corp. reported ventilation energy costs of $80 per employee, but health-care savings of $480 per employee,4 a net benefit of $400 per employee. The benefit likely was more, as respiratory infections decrease productivity well before and until long after symptoms appear.7 This indicates the importance of preventing infections.
Practical Application
The best solutions combine ventilation-effectiveness improvements and a climate-appropriate energy-recovery strategy to maximize fresh air. The engineer must balance equipment and energy costs with sick-leave and productivity savings. A ventilation rate of 52 cfm per person should decrease respiratory infections, asthma symptoms, and short-term sick leave.8
The more infectious the disease, the greater the amount of air that is required. With strongly infectious diseases, rapid improvement starts at around 15 air changes per hour (ACH); weak diseases have low infection rates at any number of ACH (Figure 2). While 20 or 15 ACH now seems impractical, one hospital study6 found outside-air rates of 16 ACH in naturally ventilated structures built from 1970 to 1990 and a median ACH of 33 in naturally ventilated structures built prior to 1950. This suggests modern mechanically ventilated buildings, with their low ACH, promote infectious disease; if that is the case, outdoor AER should be maximized with available energy-efficient equipment. In achieving its 53-percent sick-leave reduction, Polaroid went from two to three ACH. Polaroid did not consider ventilation effectiveness, which would have increased dilution further by directing ventilation air to the occupant breathing zone, reducing short-circuiting of the air.
The hospital study6 showed that for every additional 10 ACH, the chance of contracting tuberculosis goes down by about 10 percent (Figure 3). A survey of similar studies (in which ventilation was not measured directly)9 found lower ventilation rates increased respiratory-disease rates by 51 percent, to over 120 percent, and that airflows of less than 52 cfm per person8 increased the risk of SBS symptoms, increased short-term sick leave, and decreased productivity. These studies suggest the current standard of 20 cfm per person may be too low.
Figure 2 indicates benefits flow faster when ACH is above 15. If we set an ideal of 15 ACH and do the best we can with available tools, we should be able to provide excellent protection against less-infective diseases and the most feasible protection against the most infective ones. Also, we should be able to dramatically reduce air-quality problems associated with indoor pollutants.
Unfortunately, providing even six ACH can be cost-prohibitive. Most equipment, however, provides 100-percent fresh air in economizer mode, so relaxing economizer thresholds to coincide with flu season or sick-leave rates could be effective. Current practice is to engage economizers to 100-percent fresh air only when outside air is more “desirable” than inside air in terms of temperature and humidity. Health and productivity savings would raise the economizer threshold so that fresh air is “desirable” even when it is warmer or cooler than indoor air. A variable approach would reduce the energy-cost impact and make better use of expensive outside air. Otherwise, practically providing more than two to three ACH at all times using conventional HVAC requires dedicated energy-recovery equipment.
Meeting of the Minds
Organizations would do well to put human-resources (HR) managers and facilities managers, who typically do not discuss mutual cost-reduction campaigns at the water cooler, in the same boat to reduce sick-worker costs. Here is how it could work:
Facilities tasks
-
Increase outside-air flow just enough to minimize infection rates, without exceeding the cooling, dehumidifying, and heating capabilities of installed equipment. This will dilute disease-carrying airborne microbes. For new construction and major renovations, additional fresh-air-treatment equipment, energy recovery, or a dedicated outside-air system may be justified. For interior redesigns, consider dedicated ventilation diffusers.
-
Maximize ventilation effectiveness so that fresh air is used for dilution at the occupant breathing zone, rather than sent to unoccupied areas. Use computational-fluid-dynamic techniques to determine the best air-diffuser sizes and locations.
-
Reduce outside-air energy costs with: (a) energy heat-recovery technologies, (b) latent heat recovery (where appropriate), (c) passive preheating or pre-cooling of outside air with outside-air duct runs placed in ground at appropriate depth (dry climates), (d) delivery of just enough outside air only where and when it is needed, (e) occupancy- and contaminant-sensing technologies, and/or (f) tracking of outside-air-conditioning costs.
-
Minimize required hand contact with building surfaces. This will reduce disease “instillation,” or the transfer of microbes from hands to mucous membranes. Use door handles made of brass or bronze, which kill bacteria on contact, rather than plain stainless steel. Also, use push-to-open, rather than pull-to-open, bathroom doors.
-
Use germicidal ultraviolet emitters in HVAC systems. This not only will kill disease-causing microbes, it will keep coils clean and maintain coil airflow, saving energy.
-
Coordinate efforts and track results with HR.
HR tasks
-
Do not tolerate employees coming to work sick and infecting others by implementing effective policy.
-
Make leaving work as soon as respiratory-disease symptoms appear easy for employees. Do not tolerate, ”But I feel good enough to work.”
-
Adopt the Centers for Disease Control and Prevention's suggested infectious-disease measures. These concern hand-washing; eye, nose, and mouth touching; management of coughing and sneezing; and the reporting of individuals with visible symptoms.
-
Administer influenza-vaccination programs for employees.
-
Implement a sick-leave/health-care-cost tracking and evaluation program.
-
Coordinate efforts and track results with facilities management.
References
-
Epidemiologic notes and reports mumps in the workplace -- Chicago. (1988, September 9). Morbidity and Mortality Weekly Report, pp. 533-538. Retrieved from http://www.cdc.gov/mmwr/preview/mmwrhtml/00001084.htm
-
Productivity. (n.d.). Retrieved from http://biotech.law.lsu.edu/Books/lbb/x618.htm
-
Schaefer, P. (2007). The hidden costs of presenteeism: Causes and solutions. Retrieved from http://www.businessknowhow.com/manage/presenteeism.htm
-
Kumar, S., & Fisk, W.J. (2002, July). IEQ and the impact on employee sick leave. ASHRAE Journal, pp. 97-98.
-
Fisk, W.J. (2000). Health and productivity gains from better indoor environments and their relationship with building energy efficiency. Annual Review of Energy and the Environment, 25, 537-566.
-
Escombe, A.R., et al. (2007). Natural ventilation for the prevention of airborne contagion. PLoS Med. Retrieved from http://www.plosmedicine.org/article/info:doi/10.1371/journal.pmed.0040068
-
Smith, A.P. (1990). Respiratory virus infections and performance. Philosophical Transactions of the Royal Society, London B, 327, 519-528.
-
Wargocki, P., et al. (2002). Ventilation and health in non-industrial indoor environments: Report from a European multidisciplinary scientific consensus meeting (EUROVEN). Indoor Air, 12, 113-128.
-
Seppänen, O.A., Fisk, W.J., & Mendell, M.J. (1999). Association of ventilation rates and CO2 concentrations with health and other responses in commercial and institutional buildings. Indoor Air, 9, 226-252.
-
Spengler, J.D., Samet, J.M., & McCarthy, J.F. (2001). Indoor air quality handbook. New York: McGraw-Hill.
SIDEBAR: MUMPS OUTBREAK
Between Aug. 18 and Dec. 25, 1987, 116 employees at three futures exchanges in Chicago were clinically diagnosed with mumps. Three cases subsequently occurred among household contacts of affected employees. Twenty-one people developed complications; nine were hospitalized.1 Direct medical costs exceeded $56,000, with more than 700 days lost.2 The potential tort liability was significant because the mumps virus induced premature labor (which was arrested) in a pregnant employee. It is not clear whether any of the infected men were rendered sterile.
David Harlos, ScD, is an indoor-air-pollution scientist with more than 20 years of experience including governmental regulation, consulting, and university research. He served on the faculty of the Harvard School of Public Health and managed a national air-toxin-sampling network for the U.S. Environmental Protection Agency. He is an active member of the Air & Waste Management Association and the American Industrial Hygiene Association. A member of HPAC Engineering's Editorial Advisory Board, Michael West, PhD, PE, is a building-systems scientist who investigates and engineers solutions to high-energy-cost, maintenance, and comfort concerns. A recipient of the Association of Energy Engineers' (AEE's) International Project of the Year award, he has extensive experience applying renewable sources of energy and directing the development and testing of cutting-edge HVAC technologies. He is an active member of AEE and the American Society of Heating, Refrigerating and Air-Conditioning Engineers.
Did you find this article useful? Send comments and suggestions to Executive Editor Scott Arnold at [email protected].