Engineers’ Perspectives on Hospital Ventilation
Health-care HVAC design engineers are familiar with “the table,” a list of space types, pressure requirements, temperatures, and air-change-per-hour (ACH) rates. The table’s format, columns, and keynotes, as well as many of its entries, date from more than 25 years ago. In 1987, long before the era of sustainability and energy awareness in which we find ourselves, it appeared in the first edition of “Guidelines for Design and Construction of Hospital and Health Care Facilities,”1 published by The American Institute of Architects. Today, it is the responsibility of ASHRAE, which maintains the table as ANSI/ASHRAE/ASHE Standard 170, Ventilation of Health Care Facilities.
By requiring total ACH rates, the table encourages constant air volume (CAV) with reheat, perhaps the least energy-efficient central air system possible.2 The core principle—reheating, or simultaneously heating and cooling, air—is prohibited in most spaces by modern energy codes. California, for example, restricted CAV-with-reheat zones as far back as 1981.3 In the United States, unlike other countries, though, health-care spaces often are exempt.
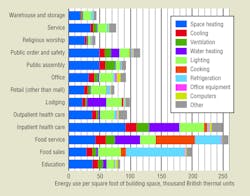
This has a significant impact on energy use. Inpatient health-care facilities are the second most energy-intensive building type in the United States (Figure 1), with heating (including reheat), cooling, and ventilation accounting for 52 percent of their energy use.4
Kaiser Permanente’s Facilities Planning & Design engineers speak with many consulting engineers about health-care design. Some consulting engineers say they feel “handcuffed” by the ventilation standard (“We could achieve so much energy efficiency, if only we could change the ventilation rates”), while others believe the ventilation rates are akin to a moral imperative (“If the code says 6 ACH, anything less endangers patients”). Wanting a better sense of these engineers’ thoughts, we conducted a survey.
Survey Design
The survey was quick and informal. A Web-based survey link was sent to 175 health-care HVAC design engineers. Names came from our address books and Web searches for certified professionals. Recipients were encouraged to forward the survey link to others. Participants were anonymous and not screened. Seventy-two responses were received.
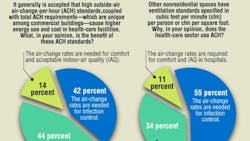
Use of the ACH convention. In two questions, we asked about the convention of specifying ACH (Figure 2). Respondents fell primarily into two camps. A substantial group (42 percent, 55 percent) said air-change rates are required for infection control. Most of the remaining group (44 percent, 34 percent) said ACH rates are not beneficial in many spaces or could be replaced by more mainstream metrics.
A minority of respondents (14 percent, 11 percent) said ACH specifications enable comfort and ensure good indoor-air quality (IAQ). In other human-occupied spaces, such as offices, schools, and churches, however, comfort and good IAQ are achieved without minimum ACH rates. In those spaces, cubic feet per minute per person, cubic feet per minute per square foot, or both are used.
Some engineers believe dilution ventilation requires ACH rates (in lieu of more mainstream metrics). We interviewed several engineers by phone before and after the survey. Several initially stated dilution ventilation, by nature, requires the use of ACH. This is somewhat concerning, as it potentially reveals a lack of understanding of dilution ventilation. (Confused? See the sidebar at the end of this article, “What Does Volume Have to Do With It?”)
For a large fraction of respondents, the ACH rates are sacred, based on infection control. Undoubtedly, patient safety is uncompromisable and must be the primary concern of hospital designers, but the connection of specific ACH rates to infection control is unclear.5,6 Many of the ventilation rates in the table, authored by consensus committees across decades, are not tied to evidence or objective research. For example, the requirement of six total ACH in X-ray (diagnostic and treatment) rooms can be found as far back as the American Society of Heating and Air-Conditioning Engineers’ (ASHAE’s) 1959 Heating and Ventilating Guide.7 There are no references in today’s standard or ASHRAE Handbook chapter indicating where it came from or on what it was based. One of the most well-known ACH rates, six ACH for patient rooms, was, in fact, based on achieving comfort,8 not infection control.
Infection control. Respondents showed sound understanding of infection-control basics (Figure 3). Through three questions, we tested knowledge of airborne-infection-control basics. Sixty-nine percent correctly answered that airflow has little or no effect on large-droplet transmission.9 Sixty-one percent answered that source control is more important than any ventilation measure in controlling environmental risks.10 Sixty-two percent correctly answered that isolation is the key to airborne disease infection control.9,11 (Within the last group, 72 percent indicated air-change rates are critical in isolation spaces; 28 percent answered they are not.)
Implications
As engineers, our challenge is to achieve safe and healthy care spaces while minimizing environmental impact.
Many engineers seem open to reconsidering health-care ventilation standards. Most, though, are wary, convinced ACH rates exist to provide infection control when, in fact, much of “the table” is based more on history and consensus than evidence.
Because engineers seem to understand infection-control fundamentals, the restrictive and prescriptive nature of the table may be unwarranted. A one-size-fits-all approach may have been appropriate when the table was created a quarter-century ago, but, today, in light of energy concerns, growing knowledge of IAQ, and ASHRAE’s commitment to sustainability, it deserves reconsideration.
References
1) AIA. (1987). Guidelines for design and construction of hospital and health care facilities. Washington, DC: American Institute of Architects.
2) Doty, S.P. (2009). Simultaneous heating and cooling—The hvac blight. Energy Engineering, 106, 2, 42-74.
3) California Building Standards Commission. (1981). California building code. Title 24, Part 2, Section 2-5329.
4) EIA. (n.d.). Commercial buildings energy consumption survey (cbecs). Retrieved from http://www.eia.gov/consumption/commercial/
5) Atkinson, J., Chartier, Y., Pessoa-Silva, C.L., Jensen, P., Li, Y., & Seto, W. (Eds). (2009). Natural ventilation for infection control in health-care settings. Geneva: World Health Organization.
6) Memarzadeh, F. (2013). Literature review: Room ventilation and airborne disease transmission. Chicago: American Society for Healthcare Engineering.
7) Hermans, R.D., & Streifel, A.J. (1993). Ventilation designs. Proceedings of the Workshop on Engineering Controls for Preventing Airborne Infections in Workers in Healthcare and Related Facilities.
8) Memarzadeh, F., & Manning, A. (2000). Thermal comfort, uniformity, and ventilation effectiveness in patient rooms: Performance assessment using ventilation indices. ASHRAE Transactions, 106 (2).
9) Siegel, J.D., Rhinehart, E., Jackson, M., Chiarello, L., & HICPAC. (2007). 2007 guideline for isolation precautions: Preventing transmission of infectious agents in healthcare settings (p. 17). Retrieved from http://www.cdc.gov/niosh/docket/archive/pdfs/NIOSH-219/0219-010107-siegel.pdf
10) CDC & HICPAC. (2004). Guidelines for environmental infection control in health-care facilities. Chicago: American Society for Healthcare Engineering/American Hospital Association.
11) CDC. (2005, December 30). Guidelines for preventing the transmission of mycobacterium tuberculosis in health-care settings, 2005 (p. 18). Morbidity and Mortality Weekly Report.
Travis R. English, PE, CEM, LEED AP, is engineering manager for health-care provider Kaiser Permanente’s National Facilities Planning group. He has more than 18 years of experience in the design and construction administration of mechanical and power-distribution systems for institutional, commercial, laboratory, and health-care facilities. His experience encompasses renewable-power systems, net-zero-building design, and building control systems.
Did you find this article useful? Send comments and suggestions to Executive Editor Scott Arnold at [email protected].
SIDEBAR: What Does Volume Have to Do With It?
Using air-change-per-hour (ACH) rates in specifying ventilation for dilution can be counterproductive. Consider the following example:
A smoke bomb is lighted in a sealed room, releasing 1 million particles of purple smoke. The room is 500 sq ft, with an 8-ft ceiling. The steady-state concentration is 250 particles per cubic foot.
Now, assume the same scenario in the same room, but with a 12-ft ceiling. When the smoke settles, the steady-state concentration is 166 particles per cubic foot.
The point is this: Contaminants naturally dilute in larger volumes. Therefore, with larger volumes, less ventilation is required for the same concentration to be achieved. When we specify a ventilation rate in ACH, we use more ventilation (which involves larger systems, more capital, more energy, more carbon emissions, and more maintenance.)
But, that is not all. The ACH metric is, itself, problematic.
When engineers say “four air changes per hour,” non-engineers hear, “The entire volume of air in the room is replaced four times every hour, or once every 15 min.” That statement is nearly true for operating rooms and unidirectional, laminar-flow cleanrooms. However, most rooms in hospitals use ceiling diffusers and return grilles; the air is mixed. A more correct interpretation is, “A volume of air equal to the volume of the room is added four times per hour.” Of course, this is difficult to say and more difficult to explain.
Still confused? Try this: Color a glassful of water deep red with food dye. Then, add a glassful of clear water. There will be spillage, but the water in the first glass still will be colored, having lightened only to dark pink. You will need to add five or six glasses (depending on the shape of the glass, the location of the pour, the speed of the pour, and other factors) before the water looks clear. For an even more fun experiment, start with red vinegar, and see how many “water changes” until you no longer can taste it.