One of the first articles I read after returning home from my most recent trip to the hospital (three operations in just over two weeks) was “Air-Treatment Systems for Controlling Hospital-Acquired Infections” (January). I must say I am pleased I read it after my hospital visits.
The article certainly was well done and gives a lot of good information. Although I have not been involved in the heating/cooling of hospitals or infection control, I was involved for many years in the control of airborne contaminants — some very toxic, demanding careful control — in industry. While it may be true that there is no relationship between reduction of hospital infections and control of industrial contaminants, can we be sure?
I was surprised the article contained little or no information about how sterile air is supplied to hospital spaces and/or how contaminated air is removed. In industry, both supply and exhaust air is used extensively in the control of airborne contaminants.
I spent several hours in a bed off the main section of the emergency room. Looking toward the ceiling, I observed what appeared to be the air supply to the space. Air was introduced through a diffuser to, I remember thinking, ensure that everyone in the space received their fair share of any contamination or infection. Later, I concluded I was wrong. The supplying of air through a diffuser surely had to have been the result of what I call We Always Have Done It That Way Syndrome.
I also had the opportunity to study the air supply in the operating room. It was through three perforated panels located in the ceiling. From my point of view, I would say: (A) the holes in the perforated metal were too large, (B) the panels were too small to provide the desired airflow pattern, and (C) the panels were not properly located to provide airflow over medical personnel and patients. Having used perforated plate in many locations where almost perfect control of airborne contaminants was required, I would say the designer had a good idea, but perhaps not the experience or the chance to install a system that would provide satisfactory airflow over the people in the room.
I believe infection control would be enhanced greatly if sterile air first flowed over all of a room's occupants, including the patient, from whom one would expect an infection to originate. The flow then would continue downward to the floor, where it would be removed from the room. Such an airflow pattern would eliminate or at least greatly reduce the circulation of contaminated air throughout the room.
I suggest that air currents be studied in full-scale hospital rooms with different methods of supplying and removing air. The use of smoke and/or bubbles should weed out air-supply systems that have no chance of controlling or reducing infections. What appear to be the best air-supply methods then could be studied further by measuring infections or determining the quantity of viruses or germs.
Kenneth E. Robinson, CIH
Mears, Mich.
Author's response:
Industrial contaminants primarily are gases and dust, while hospital contaminants primarily are microbes, so solutions can differ.
I did not address the specifics of airflow distribution because the subject is covered in existing texts and guidelines. There is, however, room for improvement in that area, as you indicated.
Although further research is needed, studies of airflow patterns in operating rooms (see my book “Aerobiological Engineering Handbook: A Guide to Airborne Disease Control Technologies,” 2006, McGraw-Hill) do not indicate any significant differences between the various airflow configurations. It appears that the highest air-exchange rates and best-possible laminar-flow distribution systems have reached a point of diminishing returns in terms of infection-reduction rates and that the solution to the problem is more complicated than simply boosting or redirecting airflow.
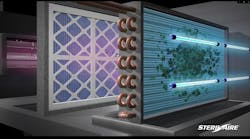
Air- and surface-disinfection systems have unexplored potential and will take us to the next level of nosocomial-infection reduction. Once widely implemented, these systems will prove to provide such significant benefits that we will wonder why we didn't adopt them 50 years ago.
Wladyslaw J. Kowalski, PE, PhD
Immune Building Systems Inc.
New York, N.Y.
Letters on HPAC Engineering editorial content and issues affecting the HVACR industry are welcome. Please address them to Scott Arnold, managing editor, at [email protected].